Abstract
Introduction: The sickle mutation of hemoglobin (HbS) afflicts millions of people worldwide and is characterized by hemolytic anemia, inflammation, painful vaso-occlusive crises, significant morbidity, and early mortality. In sickle cell disease (SCD), HbS polymerization under deoxygenation increases red blood cell (RBC) rigidity, adhesivity and susceptibility to lysis. Products of intravascular hemolysis including heme and RBC-released extracellular vesicles (REVs) promote acute and chronic inflammation triggering endothelial activation and abnormal RBC adhesion. Extracellular vesicles (EVs) are nano- or micro-particles composed of a lipid bilayer, comprised of transmembrane proteins, and enclosing intracellular remnants, including cytosolic proteins and miRNAs. EVs are known to exchange biomaterial between cells, and may serve as surrogate markers for the activated state of the parent cell thus are of high clinical significance. Quantitatively, REVs are more abundant from sickle RBCs (SS RBCs) compared with normal HbA-containing RBCs (AA RBCs). SS REVs are known to promote endothelial cell (EC) activation through cell signaling and transcriptional regulation at longer terms. However, the SS REV-mediated short term non transcriptional response of EC is unclear.
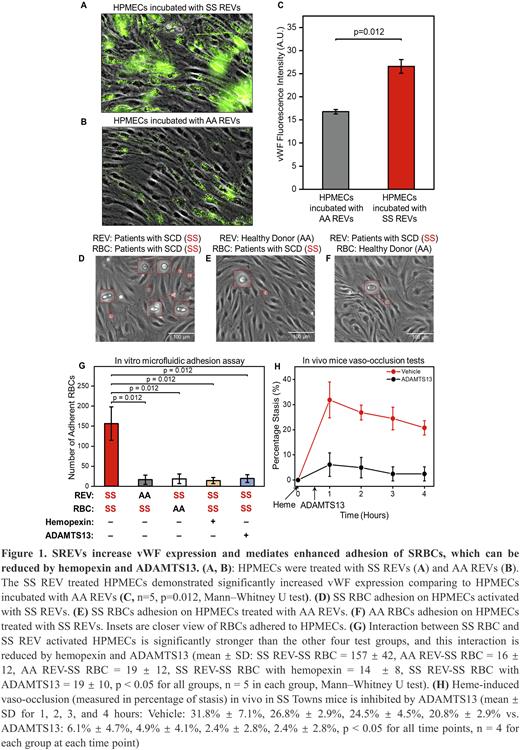
Methods: Here, we have developed the SCD-EV-BioChip using microfluidic technology. SCD-EV-BioChip assesses RBC adhesion as a biomarker for REV-mediated human pulmonary microvascular endothelial cells (HPMECs) dysfunction using functional biomarker of RBC adhesion. Utilizing SCD-EV-BioChip, Here, we examined the impact of SS REVs on acute microvascular EC activation and RBC adhesion at 2 hours. For in vitro studies, SS REVs and AA REVs were collected from pooled human SS RBCs and AA RBCs activated using calcium ionophore. The generated REVs were characterized using scanning electron microscopy (SEM) and nanoparticle tracking analyzer (NTA). HPMECs were cultured in microfluidic channels under controlled shear stress for more than 72 hours then treated with REVs at 37 ºC for 2 hours. Von Willebrand factor (vWF) expression on REVs-treated HPMECs were quantified. RBC adhesion tests were conducted with and without vWF protease ADAMTS13 and heme-binding protein hemopexin under shear stress at 1 dyne/cm2 followed by a rinse step and quantification of adhered RBCs. For in vivo study, HbSS-Townes mice and a dorsal skin-fold chamber model was used to determine if ADAMTS13 would reduce microvascular stasis in response to hemin.
Results: Within 2 hours, SS REVs, but not AA REVs, promoted increased levels of vWF expression on HPMECs, indicating HPMEC activation (Fig. 1A-C). VWF is known to trigger SRBC adhesion and vaso-occlusion. Using SCD-EV-BioChip, we found significantly increased SS RBC adhesion to HPMECs exposed to SREVs, compared to SRBC adhesion to HPMECs exposed to AA REVs, and AA RBC adhesion to HPMECs exposed to SS REVs (Fig. 1D-G). SS RBC adhesion was significantly reduced on HPMECs treated with SS REVs pre-incubated with hemopexin. ADAMTS13 is a regulator which is responsible for cleaving ultra large vWF. In this study, SS RBC adhesion was significantly reduced by vWF cleaving protease ADAMTS13 to a level similar to HPMECs treated with AA REVs (Fig. 1G). Consistent with these observations, studies in SS mice with implanted dorsal skin-fold chambers found hemin-induced stasis was inhibited by ADAMTS13 (Fig. 1F). SRBC adhesion was variable within a total of 15 test subjects with SCD, and was higher with SRBCs from patients with increased markers of hemolysis (LDH and reticulocyte count) or a concomitant clinical diagnosis of deep vein thrombosis.
Conclusions: This work demonstrated the acute, non-transcriptional contribution made by REVs to the microvascular EC activation and vWF-mediated SRBC adhesion. Results from SCD-EV-BioChip indicated the effect of hemopexin in mitigating SREV-mediated HPMEC activation. Additionally, results from in vitro SCD-EV BioChip tests agreed with in vivo stasis tests using SS mice, both of which indicated the effect of ADAMTS13 in mitigating SS RBC adhesion and vaso-occlusion.
Disclosures
Vercellotti:CSL-Behring: Research Funding; Mitobridge-Astellas: Research Funding; Omeros: Research Funding. Belcher:Mitobridge-Astellas: Research Funding; CSL-Behring: Research Funding; Omeros: Research Funding. Little:FORMA: Other: Adjudication Committee; GBT: Research Funding; bluebird: Research Funding. Gurkan:Biochip Labs: Patents & Royalties; Hemex Health, Inc.: Current Employment, Patents & Royalties; Xatek Inc.: Patents & Royalties; Dx Now Inc.: Patents & Royalties.
Author notes
Asterisk with author names denotes non-ASH members.